YMQK6PUH7QJ2
Monthly Archives: March 2011
Quotes from the Borderline
Comments from across the Borderline…
“I just want to thank you for creating this blog. It has helped me validate and understand a lot of issues I have dealt with in regard to BPD and inspired me to finally seek treatment. Again, I cannot thank you enough. I wish you the best.”
::smiles:: Thank you for such lovely thoughts. I am grateful to know that I have been able to reach out to you. You have my warmest wishes and support for all that lies ahead of you. Good luck. .
::smiles:: Thank you for such lovely thoughts. I am grateful to know that I have been able to reach out to you. You have my warmest wishes and support for all that lies ahead of you. Good luck. .
Where are all the men?: Controversy in BPD – Part 6
Discrepancy in Gender Diagnosis
 Why does it seem that men have such a low frequency of Borderline Personality Disorder? There seems to be two main reasons.
Why does it seem that men have such a low frequency of Borderline Personality Disorder? There seems to be two main reasons.1.) Men are diagnosed with something else.
2.) Men are more likely to be treated only for their major presenting symptoms.
Some studies have reported that men are more likely to be diagnosed as paranoid, passive-aggressive, narcissistic, sadistic, or with anti-social personality disorder. I’ve done a lot of research into BPD (clearly) and I’ve often come across articles that focus on BPD with ASPD. Primarily the subject study group for BPD is women, and the study group for ASPD is men. This is not necessarily an accurate distinction though.
Men and women do often present with different symptoms when you break it down to Axis I and Axis II comorbid criteria. However these symptoms are still all encompassed in the range of BPD diagnostic criteria.
Axis I co-morbid disorders:
Men with BPD tend to have higher rates of substance use disorders, while women have higher rates of PTSD and eating disorders.
There isn’t a significant difference in frequency though. These things are pretty much expected with you take into account general psychopathology/temperamental differences in gender. In things like major depressive disorder, anxiety disorders, or mood disorders there was not found to be any significant difference in BPD diagnosed gender representation.
Axis II co-morbid disorders:
There is significant difference in how men and women present in Axis II disorders which are the presentation of other personality disorder traits. Men are found to have higher rates of antisocial, narcissistic, and schizotypal personality disorders.
When you take a look at the diagnostic criteria for BPD the only real significant difference is women tend to have greater frequency of identity disturbance. Men do present slightly higher in Intense Anger and Impulsivity criteria while women tended to be a little higher in Affective instability and Avoiding abandonment.
When it comes to diagnosis between genders in BPD it was found that the function of impulsivity, how men and women tend to differ in the specific type of impulsive behavior displayed, were often different, even though the frequency was negligible. That is, Acting In or Acting Out. While women might tend towards food (internalizing behavior) men might turn towards drugs or alcohol (externalizing behavior) for self-destructive behavior. But because men tend towards externalizing it is easier to overlook the other more passive/internalized symptoms.
More aggressive acting out is likely to overshadow other symptoms that are also present. So men will be referred to anger management or therapy will focus on that particular displaying symptom, what brings it out, how to react appropriately. Or try to. I don’t know how well this works if you’re only treating one symptom and not the entire problem. Or take something like alcohol/substance abuse for example. If a woman walks into therapy and says she has a drinking problem the therapist is likely to delve into the more emotional reasons for drinking. Social stigmas for men tend to focus on the physical problem, focus on rehab and detox. They might ask what events make them want to drink and suggest how to cope with these, but not as likely to look into why they are more prone to having these reactions that cause them to imbibe in the first place.
Additionally, finding men to have higher co-occurrences of Personality Disorders is consistent with basic differences in how men and women relate to others socially. Women are socialized to be more interpersonally connected then men. A higher percentage of men with BPD also having antisocial, narcissistic, and schizotypal PDs shows increased difficulty in relatedness to others, a typical gender difference in the more pathological forms of these PDs. For example, in a sample comprised of inpatients and outpatients, men scored significantly higher on mistrust, manipulativeness, aggression, entitlement, detachment, and disinhibition, while women scored significantly higher on negative temperament, dependency, and propriety. Because the presentation of these symptoms is different, and there is a stigma towards the more passive symptom presentations, it is easier to overlook BPD as a diagnosis in favor of a more aggressive diagnosis, like ASPD for men.
All of this muddies the ability to make distinct diagnosis in men, because there may not be a distinct diagnosis for some men or they’re not being treated for their whole problem.
Maybe men should just seek psychiatric treatment more often so clinicians can get a better idea of how their PDed brains work and take some of the stigma off of us. Come on guys, help us out here. Just kidding. Sort of. ::smiles::
Female Problems: Controversy in BPD – Part 5
Myth: Only women have BPD, it’s female disorder.
That’s not to say that BPD isn’t diagnosed more often in women. It certainly is with a 3:1 ration or approximately 75% of people diagnosed with BPD are women. But men have it too. There are a lot of theories about why women are diagnosed with BPD more often:
– Sexual abuse, which is common in histories of BPD patients happens more often to women than men.
This in itself is debatable. Women tend to report these things more often, but does that mean men don’t have a similar frequency?
– Women experience more inconsistent and invalidating messages in this society.
Fortunately I think this is beginning to change, but there’s still a ways to go. And it doesn’t make up for the fact that women have been treated differently than men for most of documentable history. Especially in recent decades of greater communication women have had strong messages of how we’re supposed to act, behave, look, dress, take care of others, etc. imposed upon us… and any deviation from these cultural norms has not been met with open acceptance. We’re often told it is acceptable to be one way, but when we are it is met with negativity and sentiments of being difficult and different.
– Women are more vulnerable to BPD because they are socialized to be more dependent on others and more sensitive to rejection.
This goes along with the cultural norms imposed upon women. Personally I was taught independence to a fault, and railed against the conflicting messages of the control my parents tried to assert. I hate the idea of being dependent on anyone. Functionally, in terms of my job, my finances, the day to day aspects of my life this holds true and anyone that questions my ability to do these things is met with a rather volatile response. I hate the idea of emotionally dependent as well. I hate it. I hate it more that this is something that I can’t control when it comes to the people I get close to and involved with. The magnitude of emotional attachment that comes with BPD is part of what makes it a disorder in the first place. Becoming dependent on someone for emotional validation does make the idea of rejection so scary. Especially when there is a tendency for black and white thinking, splitting. If you do one thing wrong, you’ll lose the love and caring of that person. If they reject one thing, they’ll reject all things, and all that will be left is loneliness and abandonment. It’s not rational, but what about this disorder really is? It’s what it feels like that makes it so devastating.
– Clinicians are biased. There have been studies that show professionals tend to diagnose BPD more often in women than men, even when patient profiles are the same.
It’s not that men aren’t diagnosed with anything, their diagnosis is just different. Men tend to display symptoms differently and meet some criteria for paranoid, passive-aggressive, narcissistic, sadistic,
and antisocial personality disorders, which leads to a diagnosis of these even when BPD is a more accurate diagnosis. Since BPD has a feminine association, it’s ruled out for men almost automatically.
– Men seek psychiatric help less often.
It’s hard to diagnose someone with something when they don’t seek help for a problem. I can’t tell you how many guys I know that refuse to even go to the regular doctor when they’re ill, let alone seek therapy. I think it has to do with a culturally cultivated concept of the male ego and how men are supposed to behave. But I could be wrong.
– Men are more likely to be treated only for their major physical presenting symptoms, not necessarily the emotional associations that correspond to them. Their BPD symptoms go unnoticed because it’s assumed to be a woman’s disorder.
– Female borderlines are in the mental health system; male borderlines are in jail.
While Acting In and Acting Out are major issues for anyone with BPD, women acting out still tends to be directed towards themselves or of a magnitude that is not so outwardly destructive. Men tend towards aggression and act out towards other people leading to different consequences.
* I was incredibly destructive and explosive. I absolutely took out my problems on myself. However I constantly picked fights with my family, explosive screaming arguments, I broke down doors, put my fist through windows and walls…though these things weren’t the kind of thing that could get me thrown in jail. However, the vandalizing, drinking, shop lifting all could have.
– There has simply been very little research specifically investigating the occurrence of BPD in men.
This couples with men seeking psychiatric help less often. It’s very difficult to form a study when you don’t have a target group to focus on. It also couples with the fact that men are diagnosed and treated with potential inaccuracy so those men where BPD does present are overlooked.
So, it’s not that Borderline Personality Disorder is only a women’s disorder it’s, again, given a biased perspective. It make me sad really, that there are so many misconceptions and biases in the mental health field. It’s getting better. In the past it was taboo, not something to ever be talked about or admitted. Today it’s pretty common to seek therapy, for men and women. There’s still a ways to go though. Part of my goals for doing this blog are to increase awareness and education for Borderline Personality Disorder. I’m in no way a clinician, but I know how I’m affected, how some people in my life are affected, and I am happy to do A LOT of research to futher my own process of change. Knowing what I’m/we’re up against, options, information, treatments… simply that we’re not alone in this struggle, is encouraging. Hopefully, and it seems to be so, others find this useful as well.
Tomorrow I’ll talk more about the difference in presentation of BPD symptoms in men vs. women.
Axis I vs. Axis II: Controversy in BPD- Part 4
Where does Borderline Personality Disorder belong?
I’m referring to the DSM criteria for Axis I and Axis II designation. Let’s start off with, what’s the difference between Axis I and Axis II.
* Axis I: major mental disorders, developmental disorders and learning disabilities. Axis I disorders are predominantly mood disorders.
* Axis II: underlying pervasive or personality conditions, as well as mental retardation. Axis II disorders are personality disorders.
* Axis II: underlying pervasive or personality conditions, as well as mental retardation. Axis II disorders are personality disorders.
For or Against?
[For Axis 2] Personality disorders are classified as Axis II disorders.
Personality disorders in general have their own list of general criteria that must be satisfied. They’re a class of personality types and behaviors that the American Psychiatric Association (APA) defines as “an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the culture of the individual who exhibits it”.
“These behavioral patterns in personality disorders are typically associated with severe disturbances in the behavioral tendencies of an individual, usually involving several areas of the personality, and are nearly always associated with considerable personal and social disruption. Additionally, personality disorders are inflexible and pervasive across many situations, due in large part to the fact that such behavior is ego-syntonic (i.e. the patterns are consistent with the ego integrity of the individual) and are, therefore, perceived to be appropriate by that individual. This behavior can result in the client adopting maladaptive coping skills, which may lead to personal problems that induce extreme anxiety, distress and depression in clients.”
The behaviors cause serious interpersonal and social difficulties as well as general functional impairment. I don’t think anyone can argue that BPD fits this criteria, which is a large part of why it is considered Axis II. It also has a sub-designation as Axis II, Cluster B which is characterized by dramatic, emotional or erratic behavior. No argument there either.
Debate:
[For Axis 1] Both Axis I and Axis II are psychiatric disorders. Only personality disorders and mental retardation are segregated onto Axis II. All other psychiatric disorders are Axis I. Does it really make sense to segregate these if they are essentially the same type of thing?
[For Axis 2] However Axis I disorders are generally treatable with medication. While some presenting symptoms of Axis II disorders may be treatable with medication, it’s not shown that medication can ‘cure’ a personality disorder and correct all presenting symptoms.
[For Axis 1] Moving BPD to Axis I would have economic benefits. Many insurance companies don’t recognize BPD as a treatable condition and use it as an excuse to withhold payments. I know for a fact that my therapist classifies me as Major Depressive when billing my insurance company. I am pretty certain my psychiatrist does as well. This is certainly true, but not completely accurate. I’m not going to complain though.
I think the major debate lies here:
[For Axis 2] Axis II BPD is pervasive to a person identity, characterlogical in nature.
[For Axis 1]: But…There’s some debate about whether BPD should be considered a ‘personality disorder’ at all because it has such a high rate of co-morbid symptoms that fall into the Axis I designation.
Axis I disorders are primarily for mood disorders that are reactions to atypical situations which are not part of a person’s character. “Mood disorder is the term designating a group of diagnoses in the DSM IV TR classification system where a disturbance in the person’s mood {not their character} is hypothesized to be the main underlying feature. The classification is known as mood (affective) disorders in ICD 10.”
[For Axis 1] There are many disorders that are just as pervasive as BPD such as bipolar, anxiety, and depression that are not caused by atypical situations, and are classified as Axis I disorders.
“Two groups of mood disorders are broadly recognized (though not limited to these two); the division is based on whether the person has ever had a manic or hypomanic episode. Thus, there are depressive disorders, of which the best known and most researched is major depressive disorder (MDD) commonly called clinical depression or major depression, and bipolar disorder (BD), formerly known as manic depression and characterized by intermittent episodes of mania or hypomania, usually interlaced with depressive episodes.”
People with Borderline Personality Disorder almost always have a history of long term, pervasive depression. I’ve never heard of anyone that didn’t, but I’m not a clinician. Hypomania is not always present. If you have manic phases though, that is the definition of Bipolar and while you can have bipolar disorder and BPD, I think you would then have both Axis I and Axis II designations, not just one or the other. From here it could be argued that the mood regulation disorders are the underlying cause for all the other disorder manifestations.
[For Axis 1] There’s also the stigma that a personality disorder just means that a person has a flawed personality that can’t be changed. Except there has been plenty of research to support the idea that this is an emotional regulation disorder. Which means it would technically be a mood disorder and qualify it for Axis I.
I can see how the mood disorder aspects can affect a lot of the behaviors and symptoms of BPD. I’m not sure it can explain all of them though. Things like a tendency towards impulsive behavior, identity disturbance, fear of abandonment, etc… these are not necessarily dependent on mood alone.
I certainly don’t believe that a personality disorder just means you have a flawed personality. Calling it a flaw implies that it’s a minor issue, easily corrected. BPD is not minor, nor is it easily treatable. You might not be able to change everything about who you are (or want to), but if there is an aspect of your life that you do not value; if you are willing to put in the effort; if you have hope of living a better life or just a life different from what you currently experience– it is absolutely possible to make changes in yourself. Without hope for change there can only be resignation to the inevitable. But people do have control over their lives, what choices they make, how they want to live. It may not be easy, maybe everything can’t be ‘fixed’, but it is possible to heal from those things that we are willing to work to change.
Reinvention
The best thing about having an unstable identity is the ability to reinvent yourself however you want.
…and it confuses the shit out of everyone.
I have a request…
Dear Brain,
Please let me sleep.
Thanks,
~Management~
 Seriously. Went to sleep late. Woke up at 2am. Woke up at 3am. In a cold sweat. After mildly disturbing dreams. Didn’t fall back to sleep. Got out of bed at 6.30am. What the fuck? I was a good girl. I took my Trazadone. I don’t use stimulants in general (read: no caffeine). Why does this nocturnal phenomena elude me? Some highlights from my dream included:
Seriously. Went to sleep late. Woke up at 2am. Woke up at 3am. In a cold sweat. After mildly disturbing dreams. Didn’t fall back to sleep. Got out of bed at 6.30am. What the fuck? I was a good girl. I took my Trazadone. I don’t use stimulants in general (read: no caffeine). Why does this nocturnal phenomena elude me? Some highlights from my dream included:Saw everyone hurrying towards the exit. Apparently the building was on fire. I didn’t understand/know what was going on at first because I couldn’t hear any alarm. I strained to listen but I didn’t hear anything. I thought maybe there was a signal I hadn’t been told about. A blonde woman, maybe mid-40s looked over at me in a panic as she rushed by. I decided to go back to my desk and grab my stuff first, even though everyone else was panicked enough to leave theirs where it was. I had too much stuff and was having a lot of trouble picking it up and carrying it all. Things kept slipping. As I finally made my way out I began to see the smoke.
At some point I was picking at the palm of my hand. There were little bits of skin that I wanted to get rid of. I ended up pulling almost all the skin off of the palm of my hand until it was completely red and raw and there was a puddle of blood in my palm. I went over to the first aid kit on the far wall and got a large bandage. I knew this was something I shouldn’t let anyone see. It took me a minute to position it because I had to cut the one side to wrap it through my fingers, but it wouldn’t stay on. The EHS lady aw that I was bleeding and tried to get me to show her so she could report the injury but I refused.
I miss my apocalypse dreams. They’re way more fun.
On a lighter note. My mood has been stable since Monday. This may or may not be a good thing as I dissociated from my emotions last week and other than some self-destructive impulsive problems Thurs/Sat/Sun, they haven’t returned. I’ve been calm and ok though. I actually cannot remember any period of time in years that I’ve had more than a couple days of relatively stable moods. I’m not necessarily in a good mood, but I’m not depressed either. Calm. It’s weird. It shouldn’t be weird for steady emotions to feel odd, but it does. I don’t recognize this as a part of my existence.
Thoughts:
1.) The meds I’m on are kicking in. I do feel less depressed and less anxious. Almost not at all. However I was on these last week when I was flipping out and over the weekend when I was entertaining some destructive impulses and they hadn’t helped then. By the way, my pdoc increased my dose to 200mg/day the last time I went in to see him.
2.) I’m still dissociating from my emotions. This makes doing my therapy homework pretty difficult. I’m supposed to be writing about my emotions to cognitively recognize them as I’m experiencing them in order to form a functional connection. It’s hard to do when I’m not really feeling anything. I’m calm. It’s calming. I feel ok. I don’t know how to internalize this.
3.) I’m not in a relationship and am therefore not completely emotionally dysfunctional. Having purged or been purged from all of the dramatic factions of my friendships and relationships, with the exception of Friend – whom I no longer feel anything for, I have no drama filled emotionally turbulent external influences. Granted I also haven’t been completely alone all week so I don’t have much to compare my experimental phase to, but hey, gimme a break.
If I had to hazard a guess I’d say it was a combination of 2 and 3. My dreams seem to be a better indicator of what’s going on with me than what’s actually going on with me. Regardless, 4-5 days is good for me! Yay me. This weekend should be interesting so we’ll see how that goes.
As for tonight: Sucker Punch, bitches!
Trash talk – Controversy in BPD
Myth: BPD is a “wastebasket definition.” Clinicians give patients this diagnosis when they can’t figure out what’s wrong with them.
Janice Cauwels (1992) wrote: BPD is still a wastebasket diagnosis, a label slapped on patients by therapists trying to pretend that their illness is understood. It is also used to rationalize treatment mistakes or failures, to avoid prescribing drugs or other medical treatments, to defend against sexual issues that may have arisen in therapy, to express hatred of patients, and to justify behavior resulting from such emotional reactions.
In other words, some clinicians use the word “borderline” like some schoolyard bullies use the word “cooties.” But the fact that BPD is used as a wastebasket definition doesn’t make it a wastebasket definition, any more than calling grapefruit a fat burner makes it a fat burner. A patient should be diagnosed as borderline only if they meet the clinical criteria and only after a clinician has worked with the patient over time to verify that the BPD symptoms are persistent, extreme, and long standing”.
Basically this is more the fault of therapists. It comes about when a patient’s problems are not so clean cut and identifiable. A patient may have one or two or many problems but instead of taking the time to understand if these are separate issues the patients are thrown under the heading of BPD because it’s a disorder that encompasses such a wide range of symptoms. Actually getting to know the patient would require more effort on the therapist’s part. It’s easier to lump them under a more general category. Regardless of whether these people meet the designated criteria. Because as we know, any patient that is emotionally problematic must have a personality disorder. Dumping them under the Borderline Personality Disorder label allows them to utilize the stigma associated with BPD and dismiss them as untreatable or as a disorder that they are not equipped to deal with {read: biased against}. In short, it’s easier for the therapist to not deal with a challenging patient.
::Alternatively::
Like many clinicians, my roommate who has her M.S. in clinical psychology, describes it differently. They do not believe that BPD is an actual mental disorder. It’s not like Bipolar or Depression that is a chemical imbalance and can be quantified. She does see it as a wastebasket definition. This stems from the fact that the Borderline Personality Disorder does encompass such a wide range of problems, it’s as if any problem that cannot be explained by another disorder/diagnosis is swept together into a catch all category and filed under BPD. There is no reason that the co-morbid symptoms that comprise BPD can’t simply be separate co-morbid symptoms. For example, she’s not convinced that all of my issues don’t stem from Depression and a General Anxiety Disorder (which was the diagnosis I received from my first therapist). Except my depression and anxiety are alleviating and I still have a mess of issues.
I can understand this perspective even if I don’t agree with it. Even if it were a catchall for all these extraneous symptoms it doesn’t make it an invalid designation. Again, it provides a label that helps identify the wider range of problems that comprise the patients’ symptoms and allows for a means of recovery. Recognizing BPD as its own disorder also recognizes that these symptoms contribute to one another, compound, and are not necessarily separate entities. That there are co-morbid symptoms does not mean that these symptoms don’t stem from a common origin.
Personality disorders are tricky little bastards. You can’t quantify a personality. You can’t quantify emotional experience or relationships. All we have are our reactions and responses to the world around us. Personality is the lens through which we perceive that world. It permeates our entire being providing the means to interpret what we see and feel. Recognizing how we relate to the world around us is what allows us to function in it. For someone with a Borderline Personality Disorder, that range is expansive, so yes, it does encompass a lot, maybe too much, but then again, most days we feel too much.
A Matter of Severity: Controversy in BPD – Part 2
I thought to add this to the previous post, but I’m adding things as I find them so …. Another controversy revolves around the question:
 Without a clinical measurement of severity in personality discrepency it’s difficult to recognize where you draw the line between a healthy, relatively normal personality and something severe enough to be considered a disorder. Not only that, but who’s to say what is normal for one person is not normal for another? Unfortunately {in terms of diagnosis} people are all different so it’s nearly impossible to devise a steady measurment from patient to patient. So how do you decide on a distinguishing factor…
Without a clinical measurement of severity in personality discrepency it’s difficult to recognize where you draw the line between a healthy, relatively normal personality and something severe enough to be considered a disorder. Not only that, but who’s to say what is normal for one person is not normal for another? Unfortunately {in terms of diagnosis} people are all different so it’s nearly impossible to devise a steady measurment from patient to patient. So how do you decide on a distinguishing factor…
Is it possible to distinguish between a normal personality and a personality disorder, how do you do it, and where do you draw the line?
 Without a clinical measurement of severity in personality discrepency it’s difficult to recognize where you draw the line between a healthy, relatively normal personality and something severe enough to be considered a disorder. Not only that, but who’s to say what is normal for one person is not normal for another? Unfortunately {in terms of diagnosis} people are all different so it’s nearly impossible to devise a steady measurment from patient to patient. So how do you decide on a distinguishing factor…
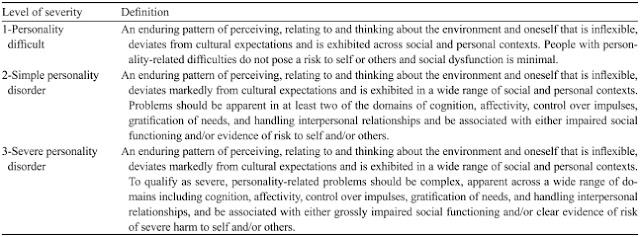
Without a clinical measurement of severity in personality discrepency it’s difficult to recognize where you draw the line between a healthy, relatively normal personality and something severe enough to be considered a disorder. Not only that, but who’s to say what is normal for one person is not normal for another? Unfortunately {in terms of diagnosis} people are all different so it’s nearly impossible to devise a steady measurment from patient to patient. So how do you decide on a distinguishing factor… “It has become increasingly clear that some form of severity assessment is necessary to decide on the priorities to use for the management of personality disorder. The notion of severe personality disorder is central to much of the work in the area of forensic psychiatry. What is clear from empirical research studies is that those with more severe personality disorder do not have stronger manifestations of one single disorder as often postulated, but instead their personality disturbance extends across all domains of personality. Although severity is not normally taken into account when classifying mental illness, it is important in personality disorders, as normal personality and personality disorder are both on the same continuum. Unfortunately, there is no measure of severity for personality disorder in the DSM or ICD classification, and the absence of these measures is of significant concern. Indeed, treatment is justified when it is likely to ameliorate distressing or disabling syndromes, even when the patients fail to meet the full diagnostic criteria of psychiatric disorders and, consequently, the measure of severity is highly relevant to the planning and provision of treatment. A reliable way of assessing personality disorder is to use 3 levels of severity (SeeTable Below). By using this measure of severity, it is possible to use the cluster system to get a measure of severity and this measure is also relevant in assessing those with the most severe personality disorders in forensic psychiatry.”
I think this ties into the idea that recognition and diagnosis of BPD is not stable. With so many different aspects and potential combinations of symptoms it’s difficult to pin point what are the distinguishing characteristics for BPD if some symptoms present, but only to a mild degree, wheras others present with much greater prominence. If something is less inhibiting should it be consider part of the dysfunction? Should only the most severe problems be included in diagnosis? Or should all manifestations be addressed and lumped together? I personally thing the 3rd is the best idea. However noting which problems are the most harmful to a persons functionality can provide a guideline for psych/therapists to map out a course of treatment addressing the most prominent features sooner.